OJ Simpson, Aaron Hernandez, Ray Rice, Kareem Hunt, Joe Mixon—the list of NFL players with histories of violence is endless. Any catalog of NFL players’ misdeeds becomes even longer if those with wayward behavior and impulse control issues are included. There’s a pretty good HBO series called Ballers that fictionally and quite hilariously chronicles some of these issues. The show implicitly attributes this to football culture and the socioeconomics inherent in taking young men from often very poor material circumstances and making them millionaires overnight.
Chronic Traumatic Encephalopathy (CTE) is a dark scientific pall that’s engulfed the NFL for decades. Maybe these surly NFL players aren’t erratic and bad with money and naturally lacking in self-control. Maybe they’re actually diseased, ailing, concussed—knocked over the head too many times. The scientific literature surrounding CTE has now been nearly 20 years in the making, and in addition to its pertinence to the NFL, it’s come to encircle the US military in the form of studying soldiers who’ve experienced concussive explosive injuries.
The new MAHA health regime has made a lot of epimethean hay out of the decades’ old failures in Alzheimer’s research. How could such an enormous amount of money have been spent on research into this ghastly disease with so little to show for it? Charles Piller has been investigating the parts that stupidity, conformity, and funding patterns have played in the field’s failures—a cliquish adoption of the languishing amyloid hypothesis of Alzheimer’s causation. Earlier this year, Myka Estes wrote a truly excellent substack series on early Alzheimer’s research and where it went wrong. This poast will be an overview of the scientific state of CTE through this lens. When you look at the scientific standards and funding patterns, the fields looks a lot like the age of amyloid in Alzheimer’s research with several shared systemic problems.
Background
The earliest scholarly work I could find about CTE is Omalu et al., 2005, which was probably the paper that created the diagnostic label of Chronic Traumatic Encephalopathy. N-grams seems to basically concur with this timeline.
When I first looked into this, I was surprised by how long ago research started on CTE-related conditions. Ten years before Omalu et al., the NFL convened a committee to examine the prevalence of “mild traumatic brain injury” in football players. Disorientation, memory loss, personality changes, aggression, confusion, and Parkinsonism don’t stay inconspicuous for long for people with large amounts of social capital like football players, and this clinical constellation didn’t tarry in being noticed by investigators. The true clinical history actually goes back to the 1940s when physicians started looking at retired boxers with obvious mental deterioration, and even that was preceded with the medical evaluation of WWI soldiers struck with “shell shock”. With the autopsy of a former NFL player, Mike Webster, Omalu et al. created a modern rebrand of much of this work as CTE.
Omalu et al. found amyloid plaques and neurofibrillary tangles (NFTs) in Webster’s brain, but not in the same anatomical pattern congruent with Alzheimer’s pathology. This is N=1 science, but you have to start somewhere; to their credit, the authors modestly conclude
This case study by itself cannot confirm a causal link between professional football and CTE. However, it indicates the need for comprehensive cognitive and autopsy-based research on longterm postneurotraumatic sequelae of professional American football. Empirical, cognitive, and postmortem data on CTE are currently unavailable in the population cohort of professional NFL players.
By this time, Alzheimer’s neuropathology documenting plaques and NFTs was nearly a century old, and the authors here were obviously quite familiar with such findings in demented brains. Interestingly, the literature seems to have moved off the idea the amyloid plaques are a strong correlate of CTE, and tau NFTs around small blood vessels are now the hallmark bioindicator in dead people. A review by Murray et al., 2022 points out tau is the most important biomarker.
… current literature suggests that the distribution and composition of p-tau and other comorbid aggregate pathologies are the most distinguishing features of CTE.
P-tau? NFTs? What does it mean?
Microtubules are essential structural components in cells. They exist inside axons, thin, elongated, little tunnels burrowing in parallel through the long part of neurons. There’s tau protein attached to the outside of the microtubules providing a type of glue-like support to the cylindrical structure and aid in assembly. In Alzheimer’s and other tau pathologies, the tau protein undergoes a transformation to a diseased state which makes holding the microtubules together more difficult. Like many pathological neuronal processes, the degenerate tau protein forms a sloppy aggregate, the NFT, that can be viewed with appropriate staining and microscopy.
Unlike in AD in which multiple independent biomarkers can be used to make a diagnosis, there are no accepted CTE diagnostic tests for living patients. This diagnostic limitation will be a major theme in the coming sections.
Scientific standards
The study of CTE has the opposite problem of Alzheimer’s science. The latter is characterized by a opaque, unknown cause leading to a terrible disease with a lot of clinical and diagnostic regularity. Neurologists are now really good at correctly diagnosing AD, even if billions of dollars of frontier research have been unable to identify a root cause or treatment mechanisms to reverse the disease.
In contrast, CTE is characterized by a completely plausible and obvious cause, head trauma, leading to clinical and diagnostic outcomes much murkier than those of AD. The careful observer will note that some putative CTE symptoms like moodiness, aggression, depression, and substance abuse are not unheard of in professional athletes or veterans, even those who didn’t play a violent contact sport like American football or get blown up by an IED, respectively.
If there’s no in vivo diagnostic test for CTE, investigators studying CTE can’t corroborate symptoms with actual biology as neurologists do with AD. They either need to use some of the potentially confused symptomatic evidence or they need to wait until the patient is dead and do an autopsy. This presents several scientific problems in CTE research.
Selection bias
In order to do autopsy-based research on a brain, you need to have someone agree to donate the brain to science. This is more likely to happen if that person was a football player or veteran or otherwise inexplicably underwent personality changes or had memory loss and their loved ones watched 60 Minutes. This can enrich data in the literature for messed up brains, no matter what syndrome actually caused a subject’s problems.
This is not an original observation, and going back to 2015, there have been meta-analyses bringing up this rather serious issue with regards to studying CTE prevalence. More recent meta-analyses agree. There’s enormous variation study-to-study in the reported CTE prevalence, with some studies reporting nearly 100% prevalence in high-risk groups. The authors conclude that this variation is most likely caused by differential brain bank profiles.
This didn’t stop breathless headlines from flowing out of Boston University’s CTE center about how practically all football players have CTE.
Confirmation bias
Once the research money and publicity get turned on, and you’ve found a putative causal link between brain pathology (e.g. NFTs) and a devastating clinical course, there are obvious incentives to continue down the path you’re on and ignore contravening evidence. If status is the currency of science, then high-impact papers are the unit of account.
Again, this is not an original observation. Asken and Rabinovici, 2021 is an extensive review of the neuroimaging methods that try to find CTE pathologies. A lot of this was quite technical, but my lay takeaway was that a majority of the measurements and methodologies used to diagnose CTE in living people produce very little signal. Differentiating suspected CTE brains from control brains is difficult even from a wide battery of neuroimaging data. Even though they don’t state this openly, this suggests researchers might be finding whatever they expect to find. This is especially true when loved ones of a deceased patient are keen to attribute their degeneration to a known syndrome. A pathologist has a lot of interpretive latitude and might use the considerable number of degrees of freedom at his or her disposal to look harder for a post-mortem diagnosis under these circumstances. They’ve improved, but even after 20 years the standards of diagnosing CTE after death are still pretty pathologist-dependent.
Blinding will help with this. Mez et al., 2017, which supplied the work underlying the aforementioned breathless headline from BU claims to have used a double-blinded clinical/pathology correlational design, so credit where it’s due. Bieniek et al., 2021 did their own blinding exercise on about two dozen brains to sharpen up the diagnostic criteria for CTE. The study is small, but they found that blinding does improve work quality compared to unblinded work. Obviously, the need for blinding is known in the field although the blinding remains inconsistently implemented.
Again, this didn’t stop breathless headlines from flowing out of Boston University’s CTE center about how practically all football players have CTE.
Small studies, bad controls
Murray et al., 2022 take the post-mortem review route and note
It is important to note that many studies had small sample sizes for the disease groups (Table 1) and groups were not age-matched in all studies
Below is an excerpt from their Table 1.
Look, I don’t want to be too uncharitable here: the best candidates for a CTE diagnosis are NFL players and veterans who’ve experienced a traumatic brain injury. We fortunately live in a society where people only experience such injuries professionally in the fields of entertainment and war. It’s pretty rare, and the people who might be willing to give their bodies to science after an early or untimely death are rarer still.
However, the sample sizes here are *much* smaller than those typically done in comparable areas of neurological research like Alzheimer’s where the datasets can be constituted of hundreds or thousands of brains.
Almost in passing above Murray et al. note the poor subject matching done when trying to control these studies. This is a complicated technical issue that I don’t want to handle rigorously here, but tau accumulation is a natural phenomenon that occurs when brains age. Subjects with suspected CTE are people who are retired from football or military service, and retired people are older than controls who might have died suddenly and randomly at a younger age and end up in brain banks. This potentially confuses the pathological analysis. Similar matching problems could exist by way of CTE comorbidities like depression, violence, and substance abuse.
Once again, this didn’t stop breathless headlines from flowing out of Boston University’s CTE center about how practically all football players have CTE.
Scientific takeaway
There are multiple technical reasons why the scientific foundation of CTE research is weak. Most of these stem from the fact no in vivo diagnostic tests exists. The good news here is that detailed reviews documenting the problems mentioned above actually exist; the issues have been pointed out by knowledgeable people in the field, not just by random anon researchers on the internet. Maybe no one will listen, but there’s no lack of reading material.
I’d never suggest CTE doesn’t exist in a clinical form or anything so extreme. There’s a lot of evidence that it does. The questions are whether the clinical presentation is causally related to the tau pathology and other physiological changes that Omalu et al. and subsequent researchers found and how common this actually is. Similarly, no one disputes Alzheimer’s disease exists, but the formerly bien-pensant explanation for the disease—amyloid plaques—is quite likely to be wrong. It’s well understood that amyloid plaques exist in normal aging brains and there’s also evidence that NFTs exist in normal aging brains with no history of traumatic injury.
Funding
Even though Omalu et al. was published in 2005, it doesn’t look like funding for CTE research got institutional traction until 2012. The NFL basically gifted $30M to the NIH to fund the study CTE, and I guess predictably this turned into a shoving match with investigations, recriminations, and acts of congress concerning how the NFL comported itself after its generosity.
From the public funding perspective, the funding series for CTE looks a lot like that for Alzheimer’s, which was growth of an order of magnitude or so from 2012 onwards. CTE funding is a little more sprawling—not limited to just the NIH but also consuming large grants from both the DoD and the VA. Today, its footprint is hundreds of millions of grant dollars. Just last month, the BU Center for CTE was awarded $15M in NIH grant money to research in vivo CTE diagnostic techniques. This was after another $15.3M less than a year before. They’ve brought in more than $32M in NIH grant money since 2021. And they brought in Matt Hasselbeck.
This seems extraordinary. I couldn’t find any definitive information about their total budget; structurally, this organization is just part of Boston University and it doesn’t have its own 990.
One way that CTE is different from other types of medical research funding is the political and PR dimensions it has via the NFL and veterans. Veterans have social capital. Football players have both money and social capital. Parties with money and social capital often engage philanthropically, and a non-trivial portion of the center’s budget is from private donations. This is no doubt true for CTE funding writ large.
Eagle and Okonkwo, 2022 seem alarmed about the extraordinary hype and lopsidedness of the media coverage and the publications surrounding CTE. There’s been a tremendous run up in public funding over the past decade. At best this hype train has led to pretty massive publication bias. At worst, it’s created a stifling monoculture like the amyloid mafia. A lot of field seems concentrated in well-funded groups with a stake in the research outcomes.
As Pillar has reported, all of this was true of the amyloid hypothesis in Alzheimer’s research, which has now been uncovered as a story of scientific misfeasance, stunted knowledge, and fraud.
Magic cures
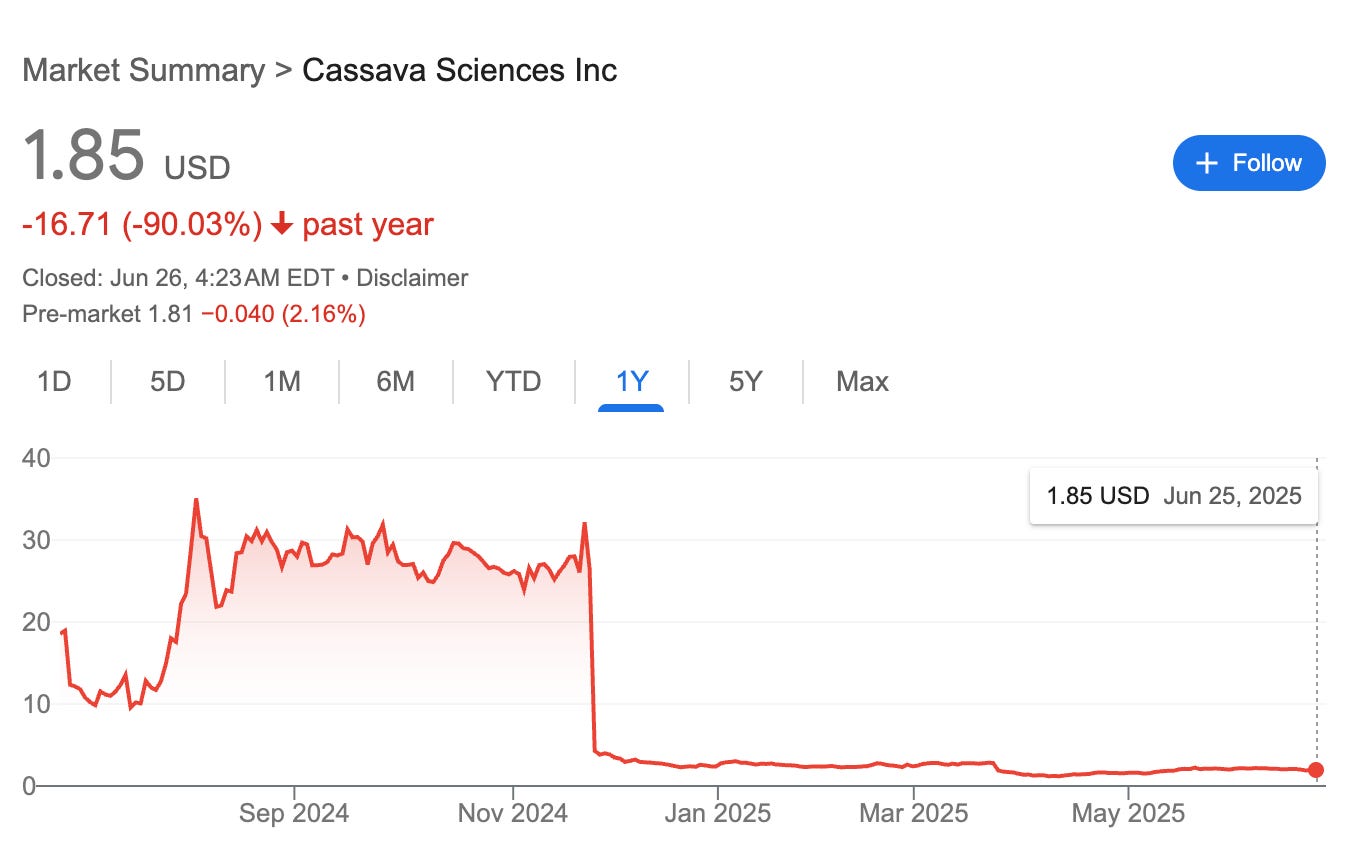
Entire enterprise units were built on the amyloid hypothesis, nearly an entire sector of the US biotech economy. The idea was simple: if Alzheimer’s disease is caused by αβ-amyloid build up in the brain, small molecule drugs that can disrupt those aggregates’ toxic interactions can reverse the disease. Cassava Science’s simufilam was such an example. Just last year, not particularly technical people deduced the drug’s phase III trial would fail from first principles. The drug failed, the company shit the bed, and one of their lead guys was actually indicted for fraud by the Department of Justice.
Biogen’s Aduhelm is a slightly less lurid case study. It’s not a small molecule, but a sophisticated monoclonal antibody designed to bind to early β-amyloid residues. It doesn’t work. In 2021, Despite basically knowing that it didn’t work, the FDA approved it for medical use in the US, leading to a scandal and several committee panelists resigning.
Biogen’s not abandoned the monoclonal antibody approach targeting β-amyloid. Lecanemab is the new and improved version. They’ve apparently smoothed things over with the FDA.
In 2013, Peter Walter discovered ISRIB, a small molecule that inhibits Integrated Stress Response (ISR) in mouse models. After they’ve been concussed or suffered traumatic brain injuries, there’s evidence that animal cognition improves. Maybe this will work in suspected human CTE subjects. Time will tell. I couldn’t find any human clinical data for CTE applications with ISRIB, but someone is probably doing it. If the small-molecule efforts in Alzheimer’s therapy are any guide to the future of CTE therapy, I’d short this stock.
Coda
No analogies are correct but some are useful. The analogy between the amyloid hypothesis and the state of CTE research is mediated by hype, technically poor science, and potentially profligate government funding. As I stated earlier, there are experts cited in this poast who have pointed out these issues, but I’m actually quite pessimistic this train will slow down soon.